Non-steroidal anti-inflammatory drugs (NSAIDs) are often the go-to option for endurance athletes seeking relief from pain and inflammation during intense training or racing. While the pain-mitigating effects of NSAIDs can seem appealing, their use in endurance sports raises significant concerns regarding performance, gut integrity, kidney function, and overall cardiovascular health. Understanding these implications is crucial for athletes looking to optimize their performance.
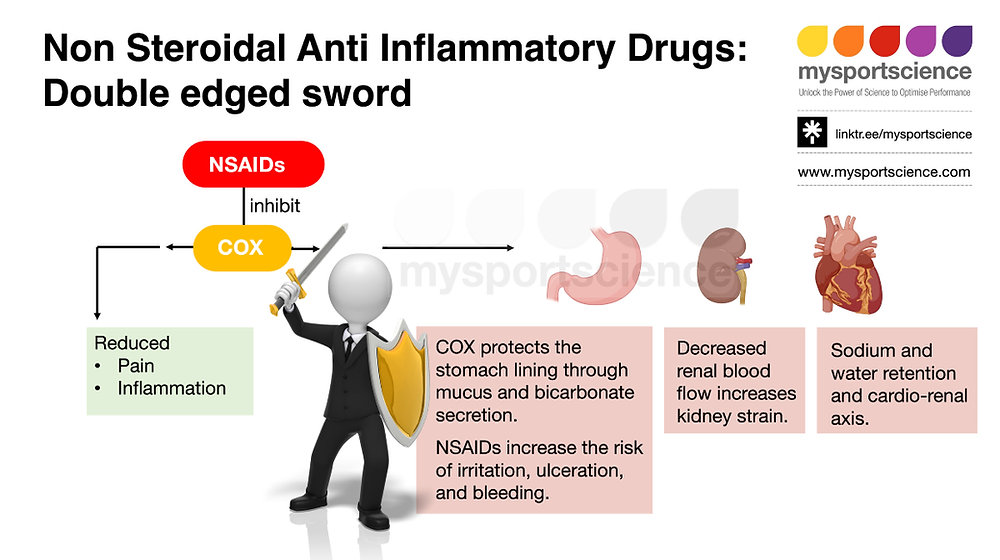
NSAIDs function by inhibiting cyclooxygenase (COX) enzymes, which play a pivotal role in the synthesis of prostaglandins involved in inflammation and pain perception. While this mechanism can mask pain, enabling athletes to push through discomfort, it also poses risks that are often overlooked, especially in prolonged exercises such as marathons or ultramarathons. Athletes may feel invincible when they can suppress pain, but what transpires within the body can be detrimental, particularly when the demands of endurance sports already strain physiological systems.
From a nutritional perspective, the use of NSAIDs has been linked to gastrointestinal disturbances. Given that endurance events can inherently burden the gut, combining exercise with NSAID consumption can exacerbate the likelihood of gastrointestinal distress, which is a prevalent cause of drop-outs and suboptimal performance. When athletes opt for NSAIDs in an attempt to stave off pain, they’re not just masking discomfort; they’re also compromising the gut’s protective barrier by inhibiting the secretion of mucus and bicarbonate. This creates a conducive environment for irritation and ulceration, making athletes who rely on these medications more susceptible to gastrointestinal complications during races.
The kidney’s ability to adequately filter waste is vital during extreme exertion. When engaged in high-intensity activities, dehydration, electrolyte fluctuations, and elevated core temperatures place significant strain on the renal system. Research indicates that NSAIDs further diminish renal blood flow, which is particularly concerning during endurance events. With compromised kidney function during exercise, athletes may inadvertently heighten the risk of acute kidney injury. It’s critical to recognize that the kidneys, already tasked with filtering metabolic byproducts arising from muscle breakdown, may falter under the additional stress induced by NSAIDs.
Another important consideration is the interconnectedness of the cardiovascular and renal systems. The so-called cardio-renal axis highlights how the strain on one may precipitate issues in the other. For instance, the usage of NSAIDs can cause fluid retention, elevating blood pressure and increasing the workload on the heart. In the context of endurance races, where maintaining both hydration and cardiovascular efficiency is paramount, the inadvertent effects of NSAIDs can lead to more severe complications like pulmonary edema and cardiac strain, hindering performance.
Data from various studies have illustrated the potential hazards of NSAID usage among endurance athletes. Instances of significant adverse events have been documented, including severe gastrointestinal bleeds, kidney failure, and cardiac complications. Despite the emphasis placed on performance enhancement through meticulous training and nutrition strategies, the adoption of NSAIDs as an “aid” fails to align with the goal of optimizing performance. Instead, it introduces an array of risks that ultimately compromise an athlete’s hard-earned efforts.
Instead of reaching for NSAIDs, athletes may explore alternative options that prioritize safety while still addressing pain or inflammation. Topical NSAIDs represent a more localized approach, allowing athletes to target specific areas without systemic absorption that compromises gut health and renal function. Other interventions, such as cold therapy, can facilitate a reduction in local inflammation, albeit requiring consistent application for sustained effects.
In addition to targeted approaches, it is essential to focus on the timing of nutrition and hydration, ensuring that athletes are optimizing these aspects without relying on pharmaceuticals. Proper fueling strategies, including the intake of carbohydrates, proteins, and electrolytes timed to both training and recovery phases, can provide the much-needed energy and mitigate discomfort without the necessity of pain-relieving drugs. Furthermore, prioritizing metabolic efficiency through consistent training can enhance the body’s ability to utilize fat as an energy source, thereby reducing reliance on carbohydrates and limiting post-exercise soreness or fatigue.
Ultimately, the goal for endurance athletes should be to cultivate robust nutrition and recovery strategies, underpinned by a deep understanding of personal tolerance and hydration needs. As training progresses and performance intensifies, the body may display signs of discomfort that signal the need for more vigilant recovery and nutrition, rather than the quick fix of NSAIDs. These signals often highlight areas for improvement, whether through adjustments in nutrition timing, hydration strategies, or recovery protocols.
One actionable takeaway for endurance athletes is to shift their focus from relying on NSAIDs for pain relief to implementing a comprehensive approach that emphasizes proper hydration, nutrition timing, and recovery strategies tailored to individual needs. Prioritize understanding how your body reacts to various training loads and leverage that knowledge to establish a robust framework for long-lasting performance without needing to mask discomfort with pharmaceuticals. In doing so, you will build resilience that not only enhances your capacity to perform at your best but also ensures sustainable health throughout your endurance pursuits.