In the realm of endurance athletics, the intricate balance of physiological systems plays a pivotal role in performance, particularly in the face of challenges presented by long-duration events. Among these complexities, understanding the mechanics of urinary continence post-prostatectomy has unexpectedly emerged as a relevant topic for those in the sport. While this might not seem immediately significant, addressing urinary incontinence can impact not just comfort but also overall performance during extended training sessions or competitions.
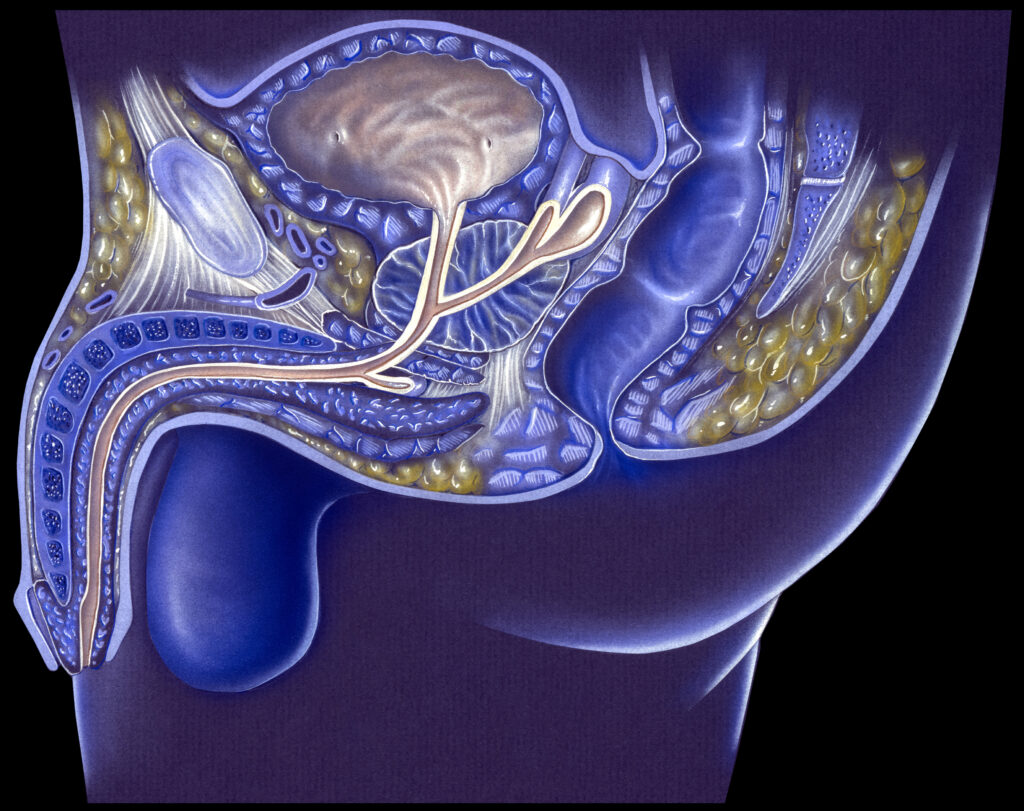
The process of maintaining continence hinges on the interplay between bladder pressure and urethral pressure. In healthy individuals, urethral pressure must exceed bladder pressure for continence to be maintained. However, in athletes who have undergone prostate surgery, there can be notable disruptions due to the surgical removal of key muscular components involved in this balance or damage to critical structures that regulate urinary control. Factors such as the loss of smooth muscle fibers integral to the internal urethral sphincter, consequent scarring, and altered bladder neck configuration can profoundly affect an athlete’s ability to manage urinary function, particularly under duress.
For endurance athletes, the vulnerability of the lower urinary tract might not be an immediate concern, yet it can manifest during high-intensity efforts or in critical racing moments, like climbing a steep ascent or navigating technical sections. The repercussions can range from discomfort to potential performance hits, particularly if an athlete becomes preoccupied with leakage rather than maintaining focus on pacing or strategy.
To counteract these issues, specific rehabilitation approaches have been developed that integrate principles of exercise science and pelvic health. These techniques often incorporate the use of pelvic floor muscle training (PFMT), which focuses not only on building strength but also on optimizing motor control and awareness of pelvic musculature. For endurance athletes, understanding how to engage these muscles—even amidst the rigors of training—can translate to improved control over bladder function, thereby enhancing focus and performance.
Fluid management is another critical aspect where mindfulness is essential. Endurance events often necessitate a delicate balance between hydration and gastrointestinal tolerance. An athlete recovering from prostate surgery may need to be particularly cautious about fluid intake, as hydration strategies that work for one athlete may not apply universally. Elevated bladder pressure from excessive fluid intake can exacerbate discomfort or urgency, undermining both confidence and performance. Therefore, fueling strategies should not only focus on energy replenishment but also consider how various nutrients might impact bladder function and gut response.
Nutritional timing also plays a crucial role in optimizing metabolic efficiency. Pre-race and during-race nutrition strategies should ideally be tailored to ensure athletes have sufficient energy without overwhelming the gut. Slow-digesting carbohydrates may be preferable for pre-race meals, while rapid-absorption options, such as gels or chews, can be employed strategically during events. Paying attention to these metabolic nuances can help prevent gastrointestinal distress—an often overlooked but significant factor for performance endurance—and contribute to more consistent outcomes in training and racing.
Supplements also warrant consideration within this context. Some studies suggest that specific amino acids, probiotics, and electrolytes may support gut health and resilience, aiding endurance athletes in their recovery and overall function. However, careful evaluation and personal experimentation are necessary to determine what may work best on an individual level, especially for those managing post-surgical considerations. Athletes are encouraged to monitor their responses to supplements, ensuring that they do not introduce variables that could disrupt gut tolerance or exacerbate urinary symptoms.
Recovery optimization is another area in which athletes should pay careful attention. This includes not only physical recovery but also a mental component, particularly for those who may be dealing with the psychological impacts of fluctuating continence. Active recovery protocols that emphasize gentle movement and proprioception can aid in both physical and psychological recovery. Utilizing techniques such as transperineal ultrasound, when appropriate, may provide feedback on muscle activation patterns and offer insights into progress, reinforcing the connection between proper pelvic muscle engagement and overall performance.
As athletes approach their training and racing schedules, the inclusion of these considerations can create a more comprehensive framework for performance optimization. It is vital for endurance athletes to maintain focus not solely on physiological training effects but also on the functional aspects of bodily systems often brushed to the side. By equipping oneself with the knowledge and tools to tailor nutritional strategies, recovery techniques, and pelvic health training, they can enhance not only their physical performance but also their overall sense of well-being.
Ultimately, one realistic takeaway is to incorporate regular pelvic floor muscle training into your routine to strengthen not only confidence in bladder control but also enhance overall core stability and power during endurance efforts. This practice could very well translate to improved focus, minimized discomfort, and more consistent performance throughout long-duration events.