Non-steroidal anti-inflammatory drugs (NSAIDs) are often utilized in the endurance sports community for their analgesic and anti-inflammatory properties, particularly during intense training sessions and races. While athletes are generally familiar with the basic benefits of these medications, understanding their biochemical mechanisms and broader impacts can provide invaluable insights for optimizing performance and recovery.
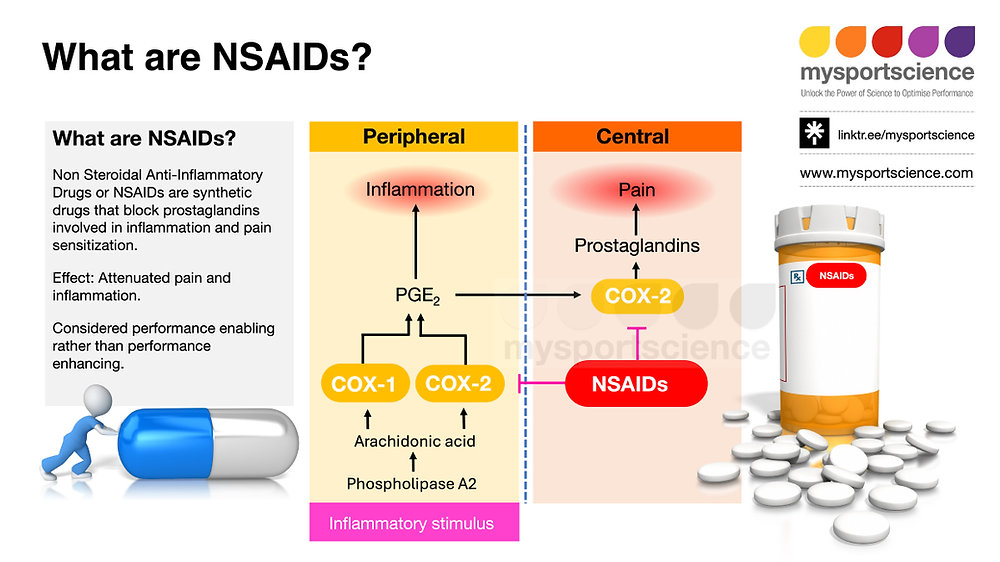
When tissues endure stress—such as during extended endurance events—an inflammatory response occurs, mediated by enzymes like phospholipase A2. This enzyme converts phospholipids within the cellular membrane into arachidonic acid, which serves as a substrate for cyclooxygenase (COX) enzymes, specifically COX-1 and COX-2. COX-1 is continuously expressed in various tissues and plays roles in protecting the gastrointestinal (GI) mucosa, regulating gastric acid secretion, and maintaining kidney blood flow through the synthesis of protective mucus and thromboxane A2, which promotes blood clotting. COX-2 is inducible and primarily activated at the site of injury. It facilitates prostaglandin production, which signals pain, inflammation, and fever.
NSAIDs exert their primary effects by inhibiting these COX enzymes, leading to a reduction in prostaglandin synthesis. This suppression helps ease pain and inflammation, which can be particularly appealing during extended training periods or competitive events. However, the nuanced understanding of how inhibition of COX enzymes affects physiological functions is essential for athletes targeting peak performance during challenging endurance pursuits.
One of the most significant considerations for endurance athletes is the impact of NSAIDs on the gastrointestinal tract, where COX-1 plays a critical role in synthesizing protective prostaglandins. During long races or training sessions, athletes often encounter gut distress, particularly when fueling with high glycemic carbohydrates or consuming large volumes of fluid. Inhibiting COX-1 through NSAID use can increase the risk of gastrointestinal bleeding and ulcers, especially when taken concurrently with high volumes of food or fluid intake. As athletes aim for efficient fueling strategies, timing becomes crucial. Rather than using NSAIDs to mask pain, a more prudent approach may involve adjusting nutrition timing and composition to minimize gut discomfort while maximizing energy availability.
Athletes should also consider the antiplatelet effects associated with the use of NSAIDs, particularly when looking to optimize blood flow and oxygen delivery to working muscles. For example, while aspirin’s irreversible COX-1 inhibition leads to prolonged antiplatelet effects, selective COX-2 inhibitors can disrupt the balance between thromboxane A2 and prostacyclin, potentially increasing the risk of thrombus formation. In the context of endurance racing, difficulty managing hydration without excessive NSAID use can lead to increased cardiovascular strain in already demanding environments, making mindful hydration strategies essential to safeguard overall health and performance.
Kidney function, another area where NSAIDs exert influence, also deserves careful consideration. Renal prostaglandins are critical for maintaining glomerular filtration rate (GFR) and are particularly important in scenarios of compromised renal function—common in older athletes or those with preexisting conditions. As endurance athletes often experience fluctuations in hydration status, particularly in longer events where dehydration can be an issue, the suppression of renal prostaglandin production through NSAID usage could increase the risk of renal complications. Athletes must balance their use of NSAIDs with thorough hydration strategies, ensuring adequate intake to maintain kidney function while still addressing discomfort that may arise during prolonged physical exertion.
While NSAIDs can provide crucial support during high-intensity training and racing, decisions regarding their use should be informed by the unique physiological requirements of endurance athletes. The potential for adverse effects is notably elevated when considering the multiple stressors involved in long-duration events, including potential dehydration, nutritional strategies, and overall metabolic efficiency. As many athletes rely heavily on their gut’s tolerance to foods and supplements during races, it may be advantageous to consider alternative methods for managing inflammation and pain, such as integrating targeted recovery protocols, utilizing cryotherapy, or employing compression garments.
In summary, the use of NSAIDs requires a balanced approach that considers not just the immediate benefits of pain relief and inflammation reduction but also the possible longer-term implications for gut health, renal function, and overall cardiovascular stability. Understanding the pharmacology of NSAIDs can significantly enhance an athlete’s ability to optimize performance while minimizing risks during training and racing, particularly in challenging environments.
To improve your endurance performance safely and effectively, assess your nutritional and hydration strategies meticulously. Focus on refining your fueling plan to foster gut tolerance while closely monitoring your hydration levels, ensuring that you maintain adequate kidney function without compromising the protective effects inherent in natural prostaglandin synthesis. This nuanced approach can bolster your resilience and enhance your overall race performance.